You are entering a field where engineering and biology meet to solve one of medicine’s toughest challenges—creating functional blood vessel networks for lab-grown organs. Without these networks, even the most advanced 3D-printed tissues cannot survive once implanted. Bioprinting vascular networks is the key step that could make fully functional, transplant-ready organs a reality.
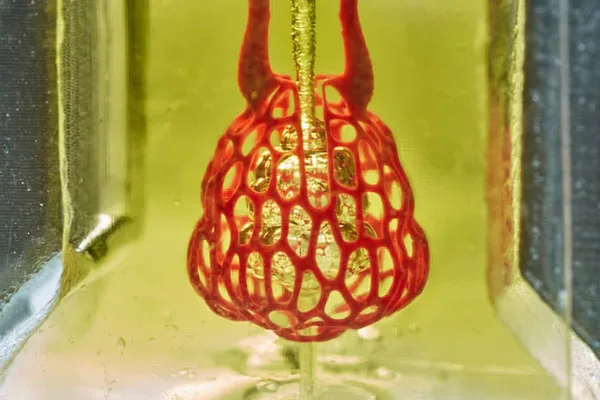
Through advances in 3D printing, researchers can now build intricate channels that mimic the body’s natural blood vessels. These structures allow nutrients and oxygen to flow, keeping lab-grown tissues alive and functioning. You gain a front-row view into how precision printing, bioinks, and tissue engineering are converging to overcome barriers that once stalled progress.
This work is not just about printing tissue—it’s about replicating the complexity of living systems. As you explore the latest breakthroughs, you will see how these developments are shaping the future of organ transplant research and moving the field closer to practical, life-saving applications.
Bioprinting Vascular Networks: Techniques and Breakthroughs
You can now create vascular structures with precision using advanced fabrication techniques, specialized bioinks, and optimized printing systems. These developments allow you to produce perfusable networks that can support nutrient transport, waste removal, and cell survival in engineered tissues.
Principles of 3D Printing in Vascular Network Fabrication
When you fabricate vascular networks, you start with a digital design that defines the geometry of channels and branching patterns. This design is then translated into a layer-by-layer printing process.
In extrusion-based methods, you can use coaxial nozzles to print hollow, lumen-containing strands. This enables the creation of continuous channels for fluid flow.
Light-based systems, such as stereolithography, let you achieve high-resolution features by selectively curing bioresins with light patterns. These techniques are invaluable when you need to work with delicate microvascular structures.
Material choice is essential. You may use hydrogels for their biocompatibility and tunable mechanical properties, or composite bioinks that combine structural support with cell-friendly environments.
Recent Advances in Tissue Engineering
You now have access to bioinks that promote angiogenesis, allowing printed tissues to develop their microvascular networks after fabrication. Growth factor–loaded hydrogels can stimulate endothelial cell migration and vessel formation.
Freeform reversible embedding lets you print complex networks within a supportive gel bath, then remove the bath material without damaging the structure. This is particularly helpful for intricate branching.
Acoustic-assisted printing can position cells with high precision, improving uniformity in vessel wall formation. Light-assisted printing has also improved speed and resolution for small-diameter vessels.
By integrating these advances, you can create constructs that better mimic the hierarchical structure of natural vasculature, from large conduits to capillary-scale channels.
Vascularized Organ Printing Methods
To print vascularized organs, you often combine direct and indirect approaches. Direct printing involves depositing bioinks in the exact shape of vessels, while indirect methods use sacrificial materials that are later removed to leave open channels.
Coaxial extrusion remains a leading method for producing continuous perfusable tubes. You can adjust flow rates and nozzle geometry to control lumen size.
Hybrid strategies combine multiple printing techniques in a single construct. For example, you might use extrusion for large vessels and light-based curing for microvascular beds.
These methods allow you to integrate vascular networks directly into organ-scale constructs, improving their viability for research and potential transplantation models.
3D print vasular networks
Impact on Organ Transplant Research and Future Directions
Advances in 3D printing of vascular networks are changing how you approach organ replacement therapies. Researchers are now producing functional tissue structures that address blood supply challenges, which are critical for sustaining complex, lab-grown organs.
Bioprinted Transplant Solutions
You can now explore transplant options that reduce dependency on donor organs. Bioprinted tissues are designed to match patient-specific anatomy, improving compatibility and reducing rejection risks.
These solutions often integrate vascular networks directly into the printed construct. This allows nutrients and oxygen to reach cells more effectively, supporting long-term viability after transplantation.
Key benefits include:
- Custom geometry for individual patients
- Reduced waiting times compared to donor lists
- Lowered immune rejection rates through personalized cell sourcing
By combining patient-derived cells with bioinks, you gain the ability to create grafts that integrate seamlessly with existing tissue. This approach is already being tested in preclinical models for liver, kidney, and heart applications.
Artificial Organ Fabrication
Artificial organ fabrication through 3D printing is moving toward producing fully functional organs with integrated vascular systems. You can now see progress in printing kidney-like structures, heart tissue patches, and liver segments capable of basic metabolic functions.
The inclusion of vascular channels is essential. Without them, larger tissue constructs cannot survive after implantation due to nutrient diffusion limits.
Researchers are refining:
- Printing resolution to create micro-scale vessels
- Bioink formulations that mimic native tissue properties
- Scalable manufacturing methods for clinical-grade production
These developments aim to make artificial organs a reliable alternative when donor supply is insufficient. While complete organ fabrication for human use is not yet routine, you can expect ongoing improvements in structural complexity and functional performance.
3D Printed Blood Vessels in Clinical Applications
3D printed blood vessels are already being evaluated for surgical grafts and tissue repair. You can use them to replace or bypass damaged arteries, or to integrate them into larger organ constructs.
Clinical-grade vessels must meet strict mechanical and biological requirements. They need to withstand blood pressure, resist clotting, and support endothelial cell growth.
Applications include:
- Vascular grafts for bypass surgeries
- Scaffold integration in engineered tissues
- Drug testing models for vascular diseases
By providing a pre-formed vascular network, you reduce the time needed for natural vessel growth after implantation. This shortens recovery times and increases the likelihood of graft survival.
If you want to advance your product development in this field, request a quote at niceandrapid.com.
